Curriculum
- 15 Sections
- 15 Lessons
- 2 Weeks
- Understanding Your Role2
- Duty of Care2
- Equality and diversity2
- Person-centred care and empowerment2
- Communication2
- Privacy and dignity2
- Fluids and nutrition2
- Awareness of mental health, dementia and learning disabilities2
- Safeguarding adults2
- Safeguarding children2
- Basic life support2
- Health and safety2
- Handling information2
- Infection prevention and control2
- Understanding learning disabilities and autism2
Curriculum
Basic life support
Learning Objective:
Understand and apply basic life support techniques safely and effectively in healthcare settings.
Assess emergency situations

In a care setting, an emergency situation is one that poses an immediate risk to the health and safety of an individual. Identifying such situations involves assessing environmental safety, checking patient responsiveness, and observing initial indicators like unusual behavior, breathing abnormalities, or sudden collapse. Before taking action, ensure the scene is safe to approach. Look for signs of distress or abnormal vital cues that require urgent attention.
- Ensure Personal Safety
- Approach Patient
- Call for Help
- Perform Preliminary Assessment
Look around for dangers such as wet floors or falling objects before approaching the patient.
Gently tap the patient’s shoulder and ask loudly, ‘Are you okay?’ to check responsiveness.
If there is no response, shout for help or call emergency services immediately.
Check breathing by observing the chest for movement; listen for breath sounds and feel for air from the mouth or nose.
Perform CPR effectively

Cardiopulmonary resuscitation (CPR) is a vital skill for healthcare providers. It involves chest compressions and rescue breaths to maintain blood circulation and breathing in an individual whose heart has stopped. Immediate and effective CPR is crucial as it sustains circulation until professional help arrives, potentially saving lives during cardiac emergencies. Remember, when performing CPR, maintain a balance between urgency and precision to ensure effective compressions and breaths.
- Compression Rate
- Compression Depth
- Rescue Breath Ratio
- Effective CPR Importance
100-120 compressions per minute.
2 inches (5 cm) for adults.
30 compressions to 2 breaths.
Maintains circulation until help arrives.
Understand use of automated defibrillators

An Automated External Defibrillator (AED) is a portable device used to treat sudden cardiac arrest. It analyzes the heart’s rhythm and can deliver an electric shock to help the heart re-establish an effective rhythm. Know when to apply the AED, as it plays a critical role in improving survival chances. Always follow the device’s safety instructions during use, primarily ensuring that no contact is made with the patient’s body while the shock is delivered.
- Safety Precautions
Ensure no one is touching the patient when delivering a shock. Stand clear and announce, ‘Clear!’ before pressing the shock button.
Manage airway obstructions effectively.

Airway obstruction, often caused by choking, is a critical condition where airflow is blocked, leading to potential oxygen deprivation. It’s essential to act swiftly to prevent severe outcomes. Initial signs include inability to speak, cough, or breathe correctly. Recognize these quickly to take immediate action to restore normal breathing and avoid harm.
- Ask if Choking
- Perform Back Blows
- Perform Abdominal Thrusts
- Seek Help if Necessary
- Explain Your Actions
- Speak Calmly
- Reassure Patient/Family
- Lay the Person Down
- Elevate Legs
- Maintain Warmth
- Call for Help
- Kneel Beside the Person
- Position Arm and Leg
- Roll and Tilt Head
- Monitor Continuously
- Danger
- Response
- Airway
- Breathing
Ask the individual if they are choking and encourage coughing if they can speak.
Stand behind the person and give 5 firm back blows between the shoulder blades.
Stand behind and make a fist. Place it above the person’s belly button and perform quick thrusts inward and upward.
If the obstruction persists, call emergency services for further assistance.
Administer life-saving interventions with empathy and respect

In emergency care, mastering technical skills goes hand-in-hand with exercising empathy and respect. While interventions like CPR and defibrillation are mechanically demanding, they should be delivered with compassionate, person-centred care. Empathy is crucial to easing patient fears and maintaining their dignity throughout the process.
Always inform the patient or their family about what you are doing and why, to reduce anxiety.
Maintain a calm tone throughout the intervention, offering reassurance.
After the intervention, take time to comfort and reassure the patient or their relatives.
Recognize and respond to shock conditions.

Shock, a critical condition caused by inadequate blood flow to organs, requires swift recognition and intervention. Look for signs such as cold, clammy skin, rapid pulse, and confusion. Early detection is crucial to prevent deterioration and ensure life-saving measures are taken promptly.
Position the person flat on their back to ensure stability.
If appropriate, elevate the legs 12 inches to improve circulation.
Cover the person with a blanket to maintain body heat.
Immediately contact emergency services for professional intervention.
Monitor and assess vital signs effectively.
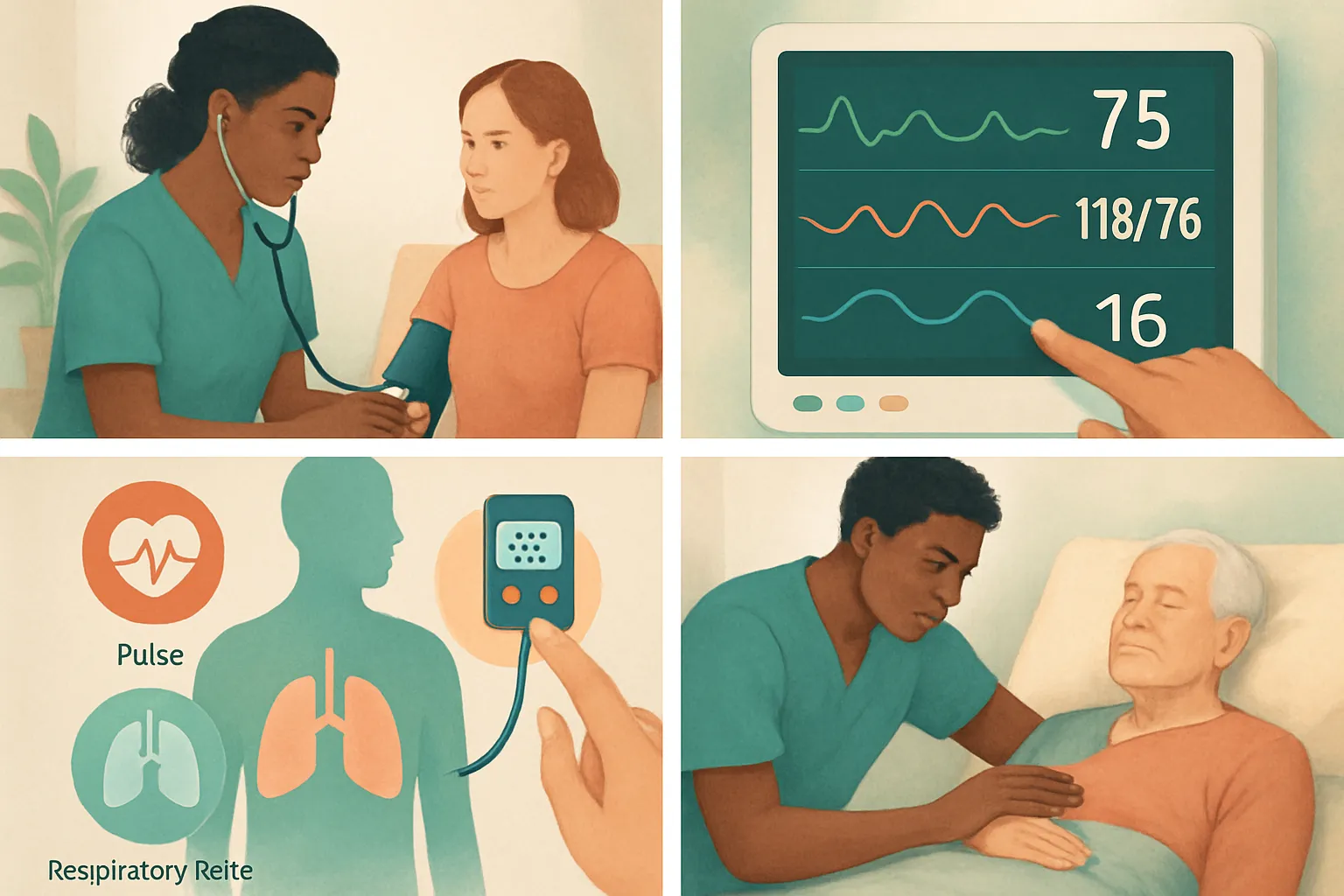
Vital signs, including pulse rate, blood pressure, and respiratory rate, are fundamental indicators of a person’s health status. Regular monitoring allows for early detection of health changes and guides timely interventions. Accurate assessment helps caregivers make informed decisions, thereby ensuring effective ongoing care.
Understand recovery positions effectively.

The recovery position is a vital post-emergency technique to maintain airway openness in unconscious but breathing individuals. It prevents airway obstruction by positioning the body safely, which allows fluid to drain from the mouth. It’s essential following interventions to ensure patient safety and stability as they recover.
Ensure clear space around the body for maneuvering.
Place the nearest arm at a right angle and cross the opposite leg over.
Roll the body onto the side and tilt the head slightly back to maintain an open airway.
Keep checking the airway and breathing regularly while waiting for help.
Primary Survey: DRABC
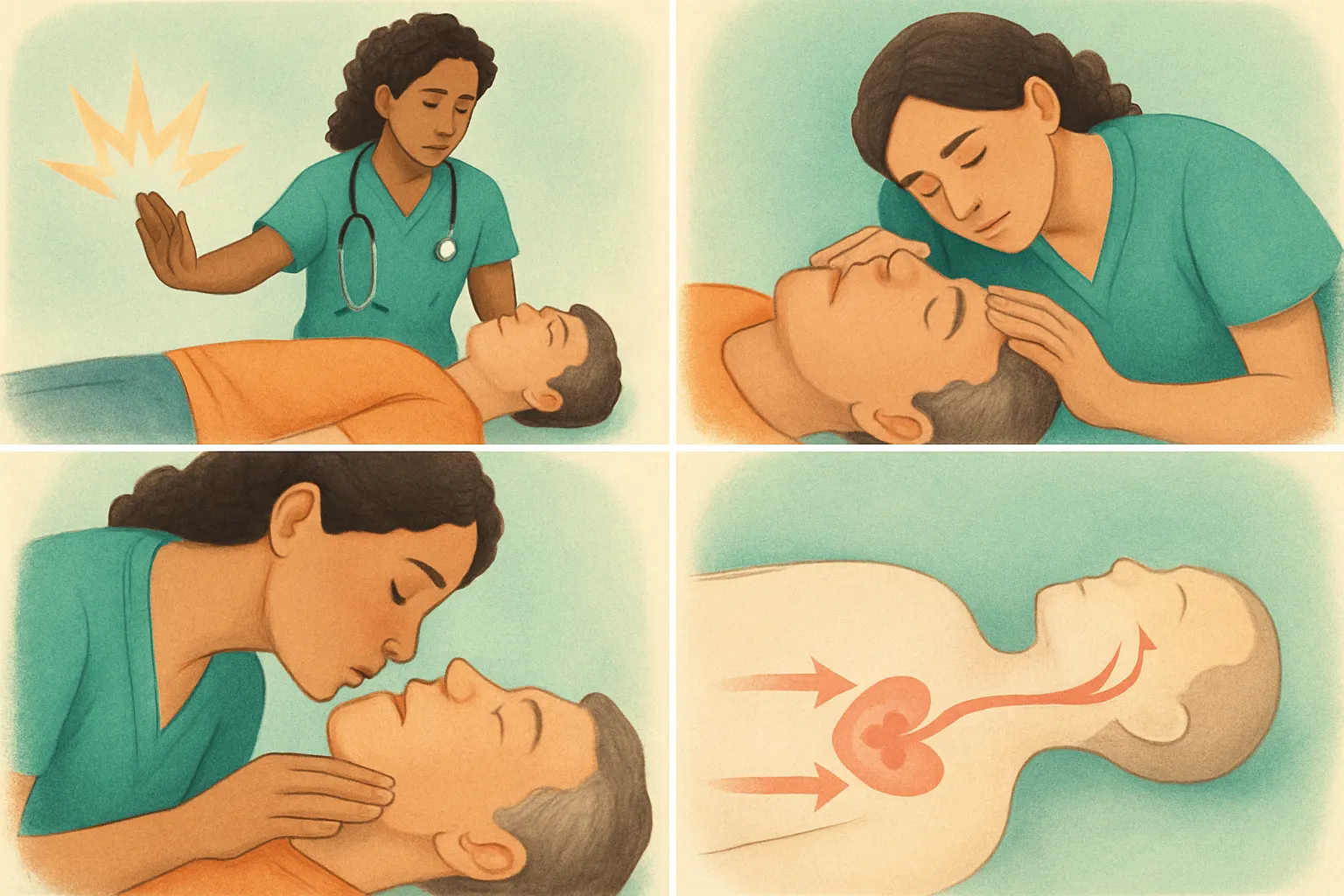
The DRABC acronym stands for Danger, Response, Airway, Breathing, and Circulation, guiding healthcare workers through a primary survey in emergencies. This structured approach ensures rapid identification and management of life-threatening conditions, increasing the chances of survival and recovery.
Assess scene safety for you and the patient.
Check patient’s responsiveness by asking and gently shaking.
Ensure the airway is open, clear obstructions.
Look, listen, and feel for normal breathing.
Understand the importance of effective teamwork in emergency situations

Effective teamwork is crucial in emergency situations, where clear communication and coordinated efforts can significantly affect patient outcomes. Each team member has a specific role, whether leading, communicating, or performing medical interventions, allowing for a comprehensive and efficient response that enhances the safety and well-being of both patients and responders.